Introduction
Chronic venous insufficiency (CVI) is one of the prevalent vascular diseases in the population. Advanced age, obesity, pregnancies, prolonged standing, positive family history, and Caucasian ethnicity are predisposing factors [1]. Several previous studies have suggested that CVI shares similar pathogenesis with varicocele in men [2, 3]. Venous valve incompetence and associated reflux, as well as venous wall pathology, are frequently proposed pathologies [4, 5].
Varicocele, found in approximately 15% of the adult male population, has been identified as the leading cause of infertility, affecting sperm count and motility in nearly 40% of cases [6]. Diagnosis is based on the palpation of dilated veins during physical examination or the visualization of dilated pampiniform veins using Doppler ultrasonography (USG).
Aim
This study investigates whether varicocele screening should be conducted in male patients diagnosed with CVI and, if so, which patients should undergo screening.
Material and methods
The study included 102 adult male patients with complaints such as burning sensation, cramps, swelling with prolonged standing, and superficial varicose veins, who presented to the cardiovascular surgery outpatient clinic between January and June 2023. Patients with a history of venous thrombosis were excluded from the study. Data were collected prospectively, and ethical approval was obtained from the Ethics Committee of Ankara City Hospital (Approval No. 3577) before the study.
After physical examination and history taking, bilateral lower extremity venous Doppler ultrasound (USG) and scrotal Doppler USG were performed. Measurements of the diameter and reflux at the junction level of the great saphenous vein (GSV) and the diameter and reflux of the pampiniform veins were taken in all patients. Reflux lasting more than 1 s at the junction level of the GSV was considered positive. The maximum GSV diameter (maxGSV) included in the analysis is based on whichever of the right GSV and left GSV diameters is higher.
According to the 2019 guidelines published by the European Society of Urogenital Radiology (ESUR) Scrotal and Penile Imaging Working Group (ESUR-SPIWG), the presence of dilatation of 3 mm or more and reflux in the pampiniform vein on either side is considered as varicocele [7].
Statistical analysis
Data from the study were analyzed using SPSS Statistics 19.0 (IBM Corp.). The Kolmogorov-Smirnov test was conducted to assess normal distribution. Descriptive statistics, including numbers, percentages, means, and standard deviations, were provided. In cases of non-normally distributed measurement data, the Mann-Whitney U test was used to evaluate the relationship between two groups, while the χ2 test was used to assess the relationship between categorical variables. ROC analysis was performed to determine the cutoff value for prediction. A type 1 error level of α = 0.05 was adopted.
Results
The sociodemographic characteristics and medical histories of the patients are presented in Table I. The mean age of the patients was 42.7 ±15.5 years. Of the patients, 37.3% were laborers, 16.7% were farmers, and 12.7% were retirees. Smoking use was reported by 57.8% of the patients. Diabetes mellitus (DM) was present in 2.9% of the patients, hypertension (HT) in 11.8%, and benign prostatic hyperplasia (BPH) in 3.9%.
Table I
Sociodemographic characteristics and medical histories of the patients
None of the patients had venous ulcers or infertility. Scrotal pain was reported by 13.7% of the patients. Right GSV reflux was present in 30.4%, and left GSV reflux in 42.2%. Varicocele was present in 34.3% of the patients. The mean right GSV diameter was 5.2 ±2.2 mm, the mean left GSV diameter was 5.8 ±2.6 mm, the mean maxGSV diameter was 6.4 ±2.7 mm, and the mean pampiniform vein diameter was 1.3 ±1.8 mm (Table II).
Table II
Clinical findings of the patients
When the relationship between demographic characteristics and varicocele was investigated, no significant relationship was found for age, smoking habits, DM or HT diagnosis (p > 0.05). However, varicocele was more common in patients with scrotal pain compared to those without it (p < 0.001).
No significant relationship was observed between maxGSV or right GSV diameter and the presence of varicocele (p > 0.05). Among varicocele patients, the mean left GSV diameter (6.6 ±2.3 mm) was statistically significantly larger than that of non-varicocele patients (5.3 ±2.6 mm) (p = 0.004) (Table III).
Table III
Relationship between varicocele presence and GSV diameters
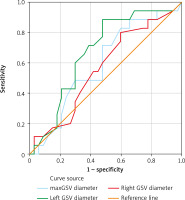
When evaluated by ROC curve analysis, both maxGSV diameter and right GSV diameter were found to have no diagnostic value for varicocele (area under the curve (AUC) = 59% and 56%, respectively, p = 0.1 and p = 0.3). In the ROC curve, the AUC for left GSV diameter was 67%, and this value was statistically significant (p = 0.005) (Figure 1).
The left GSV diameter values with the highest sensitivity and specificity in ROC curve analysis were selected for varicocele diagnosis, and in this case, the sensitivity, specificity, positive predictive value, and negative predictive value for varicocele screening are presented in Table IV. The cutoff value for left GSV diameter with the highest specificity (64.2%) for varicocele screening was 5.75 mm, while the cutoff value with the highest sensitivity (71.4%) was 5.35 mm.
Discussion
The strong association between venous insufficiency and varicocele, sharing a common etiology such as venous valve incompetence, has been previously documented in many studies [3, 8]. While varicocele is widely recognized as the most common cause of infertility in adult males, guidelines published to date have not addressed the necessity of varicocele screening in patients with venous insufficiency [9, 10].
In our study, the relationship between demographic data and varicocele was examined, but no significant association was found. However, it is not surprising that varicocele was more common in patients with scrotal pain. Furthermore, none of the patients included in the study exhibited venous ulcer findings.
According to the American Urological Association’s report on varicocele and infertility, patients diagnosed with varicocele should undergo sperm analysis, even if they do not currently complain of infertility, as they may wish to have children in the future [11]. Although none of the patients in this study reported infertility complaints, all patients diagnosed with varicocele were referred to urology specialists for examination and sperm analysis, as they were considered potential candidates for secondary infertility.
Maximum GSV diameters, measured at the junction level, from the right, left, or the higher value of the two sides, were evaluated to find a screening cutoff value. Only the left GSV diameter was found to be significantly associated with the presence of varicocele. This could be attributed to anatomical reasons, such as the left testicular vein’s 90-degree angle with the renal vein and the cross-closeness of the left iliac vein and the right iliac artery [12].
While previous studies have recommended school screenings to reduce infertility rates [13, 14], this study is the first to propose and investigate varicocele screening in patients with venous insufficiency. The shared pathogenesis between venous insufficiency and varicocele, the ease of measuring pampiniform plexus dimensions during Doppler USG examinations, and the lack of additional budget requirements make this screening feasible from a technical perspective.
The most important result of this study is that varicocele screening can be performed with 71.4% sensitivity using Doppler USG during the same session in patients with a left GSV diameter of 5.35 mm or greater, who are potential candidates for secondary infertility, azoospermia, and infertility associated with varicocele. This screening can be performed without requiring an additional budget.
Conclusions
Varicocele screening with Doppler USG during the same session can be performed without requiring additional budget resources in adult males with a left GSV diameter of 5.35 mm or greater. Both cardiovascular surgeons and radiologists can conduct varicocele screening by measuring pampiniform veins in patients with a left GSV diameter of 5.35 cm and above. This approach has the potential to reduce the incidence of varicocele and associated infertility.