INTRODUCTION
Meningiomas are the most common primary brain tumours [1, 2]. The incidence of meningiomas increases progressively with age and might be related to general diseases, e.g. neurofibromatosis type 2 and exposure to radiation [3, 4]. Ocular symptoms are mainly reported in sphenoorbital meningiomas, which are relatively rare (2-9% of all intracranial meningiomas) [5, 6] and slow-growing tumours [5]. They originate from the sphenoid bone and affect the orbit [5]. Their slow but consistent growth enables the optic canal’s infiltration and subsequent constriction of the structures within [6]. The further the growth proceeds, the higher is the risk of orbit structures’ malfunction. Hence, quicker diagnosis plays a crucial role in the treatment outcomes. The most common visual symptoms of sphenoorbital meningiomas are proptosis (45-94.6%), decreased visual acuity (30-70%), visual field deficits (14.7-30%), diplopia (2.9-15%) and orbital pain (8.6-13%) [5, 7-10]. Healthcare professionals need to be aware of the symptoms of meningiomas for the proper differential diagnosis of potentially life- and sight-threatening diseases.
CASE PRESENTATION
A 55-year-old woman complained of a black spot moving in front of her eye and a foreign-body sensation in her left eye for 3 months. The patient was referred from another ophthalmology clinic where she was seen three times, with artificial tear eye drops, eyelid margin hygiene, and vitamin A ointment recommendation, but without improvement. Potential conversion disorder was included in the differential diagnosis, and psychiatric consultation was recommended.
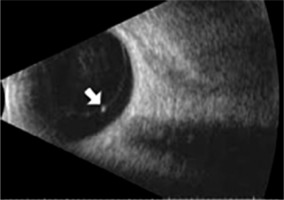
On examination there was full motility of both eyes, normal colour vision, normal direct and indirect pupil reaction to light, symmetric pupils in bright and dim light, and normal comparative visual field. The patient denied ocular pain, headache, weight loss, vomiting, and double vision. The best-corrected visual acuities were 20/20 both eyes (BE) and D-0.5 from 30 centimetres (Snellen charts) BE. Eyelids were everted and no foreign body was found. Anterior segment and dilated fundus examination revealed no abnormalities. A few vitreous floaters in the left eye were discovered and ultrasound was ordered (Figure 1). Weiss ring was identified as the possible cause of the patient’s complaints.
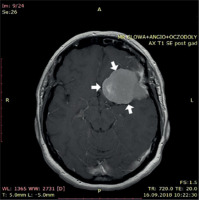
The patient returned after 3 weeks to our clinic with no improvement, still complaining of the black spot moving in front of her eye. This time visual field examination was ordered and showed a normal visual field in the right eye (RE) (Figure 2), and paracentral scotoma in the left eye (LE) (Figure 3). Next, pattern visual evoked potentials (VEP) examination showed abnormal p100 wave parameters (reduced amplitude and prolonged p100 latency bilaterally) (Figure 4). An optical coherence tomography (OCT) scan of the optic head and macula did not reveal any abnormalities. Magnetic resonance imaging (MRI) of the head was ordered (Figures 5 and 6) MRI showed a nodular, polycyclic lesion in the left frontoparietal region 54 × 40 mm, craniocaudal (CC) dimension in the sagittal projection 30 mm. The tumour was adjacent to the left internal carotid artery (ICA) and to thickened meninges of the greater wing of the sphenoid bone, causing a shift of the brain structures (Figure 5). A focal lesion of 3 mm in the right thalamus was also reported by radiologists. Neurological examination revealed no abnormalities.
Figure 4
Visual evoked potentials (Pattern-VEP 1.0 deg. Stimulator: TFT 19’’) examination showing reduced amplitude and prolonged p100 latency bilaterally at the time of diagnosis. Range of normal values in our laboratory: N75: 65-79 ms; P100: 100-116 ms, N75-P100: 7.0-26.3 μV

Figure 5
MRI examination in the frontal plane showing tumour causing a shift of the medial structures (indicated by arrows)
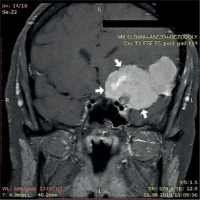
Figure 6
MRI examination (transverse plane) showing tumour causing a shift of the medial structures (indicated by arrows)
Shortly after the MRI results the tumour was surgically removed. Histopathological analysis proved a first-grade meningioma. One month after the surgery at the first ophthalmology follow-up visit the patient reported no complaints. Direct and indirect pupillary reactions to light were normal, Ishihara charts were identified correctly in both eyes, the visual field normalised, but there was a persistent swelling of the left upper eyelid (which resolved after 7 days of corticosteroid ointment treatment). Two months later, visual evoked potentials also normalised. Nine months later, the VEP result was also normal and other ophthalmologic examinations were correct, but MRI showed tumour regrowth. Radiotherapy with intensity-modulated radiation therapy (IMRT) technique to the tumour area of the lesser wing of sphenoid bone, with a dose of 5400 cGy/g in fractions of 180 cGy/g, was performed and dexamethasone tablets 2 × 1 mg were prescribed. The patient reported no ocular complaints following the procedure.
Three months after radiotherapy brain MRI examination was performed. T1, T2, FLAIR, diffusion weighted imaging (DWI), and susceptibility weighted imaging (SWI) sequences without and with intravenous contrast agent administration with axial and sagittal projections revealed maximum tumour dimensions of 29 × 20 mm. A zone of gliosis was located in the anterior pole of the left frontal lobe. The ventricular system was located medially and pericerebral fluid reservoirs were preserved. Five years after surgery, annual ophthalmologic examination detected no significant changes in vision and no ocular complaints.
DISCUSSION
Ophthalmic symptoms dominate as the first symptoms that patients with sphenoorbital meningiomas complain of [5]. The symptoms, however, usually are unspecific and imprecise, suggesting further diagnosis of meningioma. Proptosis (45-94.6%), decreased visual acuity (30-70%), visual field deficits (14.7-30%), diplopia (2.9-15%), and orbital pain (8.6-13%) predominate [5, 7-10].
Our patient was unique because the most prominent problem was an isolated scotoma, which can be present in a variety of ophthalmologic disorders. Moreover, coexisting floaters might mimic scotoma and falsely reassure the ophthalmologist with an inappropriate benign diagnosis [11]. Both the patient’s history and ultrasound examination findings resulted in the initial misdiagnosis. This delayed proper management and a surgical intervention, which is known to worsen the long-term prognosis of the patient’s visual function [12].
The surgery itself is a key factor that improves the visual status of the majority of patients (57% according to one study) [6]. Properly performed neuroophthalmological examination can also serve as a determinant of postoperative visual recovery. The duration of symptoms, preoperative visual status and tumour size have the most statistical significance for the visual outcome of the meningioma surgery [13]. The visual outcome after the procedure was more favourable for patients with symptoms present for less than 2 years [6]. The prognosed vision status of patients with tumour size less than 3 cm in its maximum diameter and without concentric invasion of the optic canal was statistically significantly better [6, 13]. Additionally, the vision of patients with a thin peripapillary retinal nerve fibre layer (RNFL) (5379 μm) determined on OCT was less likely to improve [14]. However, macular ganglion cell complex thickness in nasal quadrant was found to be most reliable for assessing the chances of post-surgical visual field improvement [6]. Concerning VEP’s importance, a significant decrease in amplitude serves as a valuable marker of the optic pathway’s compression as well as a prognostic factor for future improvement [6]. A large body of evidence proves that neither age nor sex affects expected visual outcomes significantly [13]. However, some studies have shown that age of over 65 years may be correlated with faster regrowth of the tumour [15].
Follow-up management is a multidisciplinary challenge which should consist of regular appointments involving both visual acuity tests, as well as ancillary tests [16]. OCT scans can also be useful to assess the thickness of the RNFL (thickness of less than 70 μm can be a negative prognostic factor for reoperation) [14, 17]. Magnetic resonance imaging of the head is used to control the size and pace of the potential regrowth of meningioma [18]. The proper frequency of ophthalmological examinations is not certain. In one study, visual acuity testing and visual field testing were performed within 1 week of surgery, then at 3 months and every 6 months thereafter; connected with previously mentioned optical coherence tomography it could serve as a possible algorithm for ophthalmologists [13]. In other study postoperative ophthalmic examinations were recommended at 1 month, 6 months and 1 year after the procedure [16]. In the case of our patient, she visited the ophthalmology clinic one month after surgery for visual acuity and visual field examination. Two months later, there was another follow-up visit, three months later, another one with visual evoked potentials and visual field examination, seven months later, another visit with all of these examinations showing proper results. However, MRI performed the next day showed tumour regrowth. This could suggest that MRI should serve as a priority examination in further management of meningioma patients and we should not rely only on ophthalmological symptoms and signs, which might be absent even in progressive regrowth. However, ophthalmologic examinations of choice and key symptoms in a follow-up management of patients after sphenoid meningiomas’ removal should be further investigated.
CONCLUSIONS
Ophthalmic symptoms dominate as the first clinical symptoms of sphenoorbital meningiomas. This case emphasises the importance of understanding the symptoms reported by our patients. The black spot was misdiagnosed as a floater instead of a potential scotoma. Properly performed neuroophthalmological examinations, supported by ancillary testing, e.g. OCT, visual field, VEP and MRI, aid our clinical differential diagnosis and follow-up.

 POLSKI
POLSKI