Coronary artery anomalies encompass a diverse and intricate group of congenital disorders, exhibiting variations in manifestations and underlying pathophysiological mechanisms. The understanding of coronary anomalies has evolved significantly, encompassing aspects such as their definition, clinical presentation, diagnostic evaluation, prognosis, and treatment approaches [1]. Identifying these anomalies and recognizing the associated functional impairments pose a significant challenge. To comprehend the clinical implications of these anomalies, it is crucial to elucidate and ascertain the mechanisms that disrupt the normal functioning of the coronary artery, resulting in inadequate blood supply to the dependent myocardium [2].
In this case report, we present the case of a 58-year-old man with a fistulous connection between the pulmonary artery (PA) and the left main (LM) coronary artery. The patient sought medical attention from his cardiologist due to experiencing typical stable angina symptoms during mild exercise. Initial evaluations, including electrocardiography (ECG) and echocardiogram, did not reveal any pathological findings. As a further investigative step, cardiac magnetic resonance imaging (cMRI) was recommended. However, even cMRI did not identify any pathological abnormalities. Despite the absence of detectable findings, he continued to experience persistent and worsening symptoms. Consequently, the patient was referred to the cardiology department at Westpfalz-Klinikum for coronary angiography. The performed angiography revealed mild atherosclerosis without any significant stenosis. However, it also uncovered the presence of an additional vessel connecting the LM to the PA (Figure 1). This additional vessel caused a steal phenomenon, diverting blood flow from the LM towards the PA, leading to clinical manifestations of angina. Due to the extremely narrow ostium, interventional occlusion of the fistula was not feasible. As a result, the patient was subsequently referred to our department for surgical intervention. During the intraoperative examination, the additional vessel was identified, coursing posteriorly around the main PA (Figures 2 A, B). Utilizing cardiopulmonary bypass (CPB), the PA was opened at the level of the pulmonary valve, and the fistulous communication was located in the region of the left leaflet. The fistula was then ligated on both sides of the PA wall (Figures 2 C, D). The intraoperative course proceeded without any complications, and the patient was successfully weaned off CPB without any issues. Postoperatively, the patient was transferred to the intensive care unit. Extubation was performed 3 hours after the surgery’s completion. On the second postoperative day, the patient was transferred to the clinical ward, and the rest of the postoperative period transpired without any noteworthy events. Ultimately, he was discharged from the hospital on the 8th postoperative day, remaining free of any angina symptoms. During the 1-month and 3-month follow-up appointments, the patient remained asymptomatic.
Figure 1
A, B – Coronary angiography shows the fistula between the left main artery and the pulmonary artery
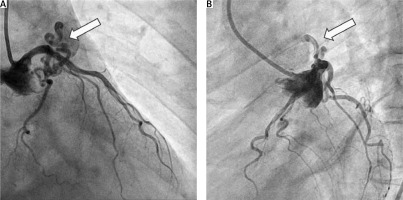
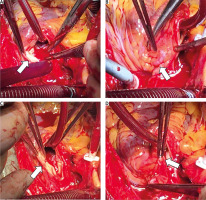
Figure 2
A – Identification of the ostium of the fistula at the level of the pulmonary valve. Continuous bleeding is observed despite cardiopulmonary bypass with cardioplegic arrest. B – Visualization of the course of the fistula around the pulmonary artery. C – Ligation of the ostium of the fistula at the interior wall of the pulmonary artery using a 5-0 polypropylene suture. D – Occlusion of the fistula at the exterior wall of the pulmonary artery using a vessel clip.
A coronary artery fistula (CAF) refers to an abnormal connection between a coronary artery and the chambers or major vessels of the heart. The first description of these abnormalities, by Krause, dates back to 1865 [3]. Typically, CAFs are congenital in nature, although in a small percentage of cases, they can be acquired abnormalities [4]. Traumatic cardiac injuries commonly give rise to acquired CAFs, while iatrogenic CAFs are typically associated with interventional or surgical cardiac procedures [5, 6]. In cases of traumatic coronary artery-cameral fistulas, which are rare consequences of trauma, early surgical intervention is necessary to prevent complications [6]. There are two main types of CAFs: coronary-cameral fistulas, which establish connections between coronary arteries and any of the heart chambers, and coronary artery malformations, which form connections between coronary arteries and systemic or pulmonary vessels [5]. CAF is an extremely uncommon anatomical abnormality, occurring in approximately 0.002–0.9% of the general population. However, the prevalence increases to 0.25% in patients undergoing coronary angiography [5, 7]. CAFs can originate from both the left and right coronary arteries, with the right coronary artery (RCA) and the left anterior descending (LAD) coronary artery being the primary sources of the majority of these fistulas. Involvement of the circumflex coronary artery is infrequent. CAFs originating directly from the LM are very rare and account for less than 5–35% of cases [8]. Regarding drainage, most CAFs drain into the right side of the heart, while less than 15–17% drain into the PA [8, 9]. Limited case reports have described coronary-pulmonary arterial fistulas (CPAFs), which are uncommon anomalies affecting the coronary arteries. Verdini et al. conducted a comprehensive investigation involving 103 patients with CPAFs, to identify prevailing patterns or common characteristics [10]. The main termination site of the fistula was observed to be the main PA in the majority of cases (89%). Multiple CPAFs were detected in 45% of cases, and coronary artery aneurysms were found in 19% of cases. Pediatric CPAF cases often exhibited an association with pulmonary atresia accompanied by ventricular septal defect [10]. Cai et al. [11] reported a prevalence of CAF of about 0.5% in coronary computed tomography angiography (CCTA) cases. Among the various types of CAF, CPAFs exhibited the highest incidence, whereas left ventricular fistulas were more frequently observed in coronary-cameral fistulas (CCFs). In comparison to CPAFs, CCF fistulas tended to be associated with a larger diameter of draining, larger aneurysms, and a single fistula pattern [11]. More than half of patients with CPAF exhibited no related symptoms [12]. The clinical symptoms are attributed to the “coronary steal phenomenon”, which can lead to symptoms such as angina or dyspnea even in the absence of stenosis [13]. The term “coronary steal” emerged in 1967 as a vivid description, drawing a parallel to the term “subclavian steal” introduced in an editorial in 1961 [14, 15]. Both terms employed the concept of “steal” to depict flow reversal within an interconnected yet abnormal vascular network [15]. The fistula between the LM and the PA establishes continuous flow throughout the cardiac cycle, with direction from the LM to the PA [2]. Elevated-pressure blood flow from the coronary arteries, as it drains through a low-resistance venous circuit via the fistula, bypasses the smaller arterioles and capillaries within the myocardium. Consequently, regions downstream of the CAF may experience inadequate perfusion [2, 5]. The severity of these effects depends on factors such as the resistance characteristics (length, size, and tortuosity) of the fistula and the specific location of its connection. The resulting consequences may manifest as dyspnea, angina, myocardial infarction, or signs of volume overload [5]. However, most patients remain asymptomatic throughout their lifetime. Small fistulas do not significantly impact patients’ hemodynamic profile, while larger fistulas may present with clinical manifestations of angina, dyspnea, pulmonary hypertension, or heart failure [7]. In the coronary-pulmonary arterial fistula (CPAF) case series by Verdini et al., the primary reported symptoms were chest pain (39%) and dyspnea (25%). Notably, a murmur was the most frequent finding during physical examination (37%) [10]. Arrhythmias, such as polymorphic ventricular ectopy, have also been reported [5, 13]. Most abnormalities of the coronary arteries are incidentally detected during coronary angiography [4, 5]. CCTA is however considered the gold standard for diagnosis today [9]. CCTA is a valuable and noninvasive imaging modality for identifying CAFs [11]. Its utility is particularly notable in detecting small fistulas and providing surgical guidance for complex CAF cases. Among a total of 10,121 cases of coronary CT angiography conducted over a span of 7 years, Lee et al. [12] identified 32 cases of CPAFs. All detected CPAFs followed an anterior course toward the main pulmonary artery and drained into its anterolateral aspect. Notably, the CPAFs observed in this study frequently exhibited aneurysmal alterations [12]. Additionally, MRI can provide useful information regarding CAFs. Transesophageal and transthoracic echocardiography are useful in assessing the hemodynamic parameters of CAFs [7]. The management of CAFs depends on their size and symptoms [9]. The main indication for closure is the development of symptoms of heart failure and myocardial ischemia. Small, asymptomatic CAFs can be managed conservatively with appropriate medical treatment and should be monitored every 3–5 years [16]. Larger CAFs, even if asymptomatic, should be closed either percutaneously or surgically. According to guidelines provided by the American College of Cardiology and the American Heart Association, surgical intervention is strongly recommended (Class I) for large CAFs regardless of symptomatology. Surgical management is also recommended for symptomatic small to medium-sized fistulas. The available treatment options include surgical ligation, which can be performed via either epicardial or endocardial ligation techniques [5]. It is typically recommended for large high-flow fistulas, as well as for fistulas that are tortuous, have multiple communications and drainage sites, or display large aneurysms. Surgical ligation becomes a viable choice if simultaneous distal bypass grafting is required [5]. Transcatheter intervention is suitable only in cases where the morphology is simple, and the choice of the closure device is based on the anatomical characteristics of the fistula [9]. Interventional coiling is also an option [13]. Therefore, in cases of CAFs with a proximal origin, a single draining site, non-tortuous characteristics, extra-anatomic terminations, absence of comorbid cardiovascular disease, or involvement of older high-risk patients, percutaneous transcatheter closure should be considered [5]. Patients treated through transcatheter intervention or surgery have a good prognosis. Recurrence rates are around 9–-19% for transcatheter closure and 25% for surgical ligation. Echocardiographic follow-up is necessary 1 month after the procedure [2]. The long-term outcome of CAFs is not fully known due to their rare incidence and wide variety of manifestations. Wada et al. reported no deaths, significant ST changes, or events associated with CAFs during a follow-up period of 66.2 months after surgical repair [17]. Long-term outcomes of surgical repair demonstrated satisfactory results, indicating that concurrent intervention for CAFs during surgery for coexisting cardiac conditions is beneficial in mitigating potential future complications associated with CAFs [17]. Additional studies with an increased sample size are warranted to assess the long-term outcomes associated with various treatment procedures for CAFs.
This study highlights the critical importance of performing comprehensive and meticulous evaluations for patients exhibiting symptoms of angina. The clinical presentation of these disorders closely mimicked coronary artery disease, thereby presenting a significant diagnostic challenge. Moreover, our case emphasizes the difficulty in diagnosing such disorders. Although these disturbances are rare in clinical practice, it is imperative to foster a heightened clinical suspicion for timely recognition and accurate diagnosis, enabling the implementation of appropriate management strategies. This emphasizes the need for future healthcare practitioners to maintain vigilance in identifying similar entities, ensuring prompt and effective management.





