Introduction
Myeloproliferative neoplasms (MPNs) are a heterogeneous group of hematologic disorders characterized by clonal proliferation of myeloid lineage cells. Depending on the type of MPN, the process leads to an increased number of one or more types of blood cells. The incidence rate of MPNs in Europe is relatively low and is estimated at about 3.1-3.3 for 100,000 people [1, 2].
Giant cell arteritis (GCA) is one of the most common vasculitides in medium-aged and elderly patients. However, it is also rarely diagnosed with up to 30 cases/100,000 people older than 50 years [3]. The disease affects medium and large vessels, typically the aorta with its branches and cranial arteries. GCA is often associated with musculoskeletal inflammatory disorders such as polymyalgia rheumatica (PR) [4]. Treatment is usually based on corticosteroids and other immunosuppressive agents.
Co-incidence of MPNs and autoimmune diseases has been quite widely reported in the literature, mostly in patients suffering from myelodysplastic syndrome and chronic myeloid leukemia (CML). Pathogenesis of the co-occurrence is not well known; however, the association of those entities is noticeable.
In our paper we would like to present a case of a patient diagnosed with unclassified MPN and GCA treated with allogeneic hematopoietic stem cell transplantation (allo-HSCT) which resulted in the remission of both diseases.
Case report
A 60-year-old man was admitted to the Hematology Department in March 2017 due to high leukocytosis. The patient suffered from weakness and generalized musculoskeletal pain which had begun a few months before admission. In physical examination only slight hepatomegaly was found. Laboratory tests revealed an increased C-reactive protein level (173 mg/l) with negative blood and urine cultures, white blood cell (WBC) count 48 × 103/µl and mild anemia due to iron insufficiency. In blood smear segmented neutrophils and band forms accounted for 70.5% of WBC, maturing neutrophils 17%, monocytes 5.7%, basophils 0.3% and blasts 3%. In the bone marrow biopsy hypercellularity, slight reticulin fibrosis (MF-1), megakaryocytic and granulocytic proliferation with no dysplasia in granulocytic lineage cells and slight dysplasia in megakaryocytic lineage cells were found. Bone marrow smear evaluation revealed 3.5% of myeloblasts, 90% of myeloid lineage cells (including 43% of maturing neutrophils), and dysplastic features in less than 10% of granulocytic lineage cells. As the laboratory results indicated myeloproliferative neoplasm, further diagnostics involved the evaluation of typical mutations in MPNs such as BCR-ABL1,JAK-2, CALR,MPL,PDGFRB,FGFR1,del7q,MLL5,EZH2,MYH11,CBFB with negative results for all of those.
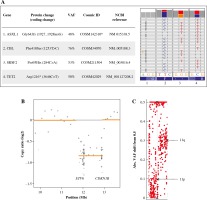
Since no classical driver mutation described in MPNs was found using classical cytogenetic and molecular methods, targeted next-generation sequencing (NGS) was applied (Supplementary file with materials and methods). Briefly, we employed a custom-designed panel (SeqCap EZ Choice XL by Roche) covering almost 10 MB of exonic regions of more than 1000 cancer-associated genes Supplementary Table 1. After filtering (as described in the Supplementary materials and methods file), out of 44 rare variants, 4 top-scoring clinically relevant mutations were identified, namely in ASXL1, CBL, SRSF2 and TET2 genes (Fig. 1A). All of them are typical mutations in myeloid malignancies. ASXL1 and TET2 are also the most frequently mutated genes in atypical chronic myeloid leukemia (aCML) as described recently by Tefferi’s group [5]. According to this work, mutations in TET2 have additionally prognostic significance. Moreover, copy-number variants (CNV) analysis (Supplementary materials and methods) revealed focal deletion in chromosome 12 affecting ETV6 and CDKN1B genes (Fig. 1B), previously described in acute myeloid leukemia (AML) with complex karyotype (Supplementary materials and methods) [6] and T-cell prolymphocytic leukemia [7]. Also copy-neutral loss of heterozygosity was detected in chromosome 11 (Fig. 1C) affecting the CBL gene, which explains higher variant allele frequency (VAF) for the mutation identified in CBL (76%). Such genetic events were previously described in clonal evolution of myelodysplastic syndrome (MDS) [8] as well as in chronic myelomonocytic leukemia (CMML) [9]. Observed alterations confirm a complex genetic picture of this case and do not allow it to be unequivocally classified.
Fig. 1
Relevant genetic aberrations detected by NGS in patient’s sample. A) Mutations in ASXL1, CBL, SRSF2 and TET2 genes, presented as screenshots from IGV. *Provided is an ID of an ASXL1 mutation which arises from insA instead of G but results in a similar frameshift. VAF – variant allele frequency. B) Focal deletion on chr12 detected in sequencing coverage analysis, resulting in monoallelic loss of locus containing ETV6 and CDKN1B. C) Allele frequencies of common variants detected on chromosome 11 in patient sample. Each point of the chart represents VAF of a single variant. VAF shift on 11q arm suggests a loss-of-heterozygosity event
Differential diagnosis included such types of MPNs as aCML, CMML and chronic neutrophilic leukemia (CNL) and was performed according to the WHO 2016 MPN Classification. Criteria for none of the above-mentioned diseases were fully met. Together with the results of NGS analysis, this led to the diagnosis of unclassified MPN (MPN-U).
Increased inflammatory parameters without features of active infection and persistent polymyalgia suggested co-occurrence of rheumatic disease. In laboratory tests, ANA1, ANCA, anti dsDNA, anti Scl-70, anti-endomysium, anti-transglutaminase, anti-gliadin antibodies and rheumatoid factor (RF) were negative. Due to suspicion of seronegative autoimmune disorder, the further diagnostic process included positron emission tomography (PET), which revealed involvement of the ascending aorta, aortic arch and its large branches characteristic for GCA.
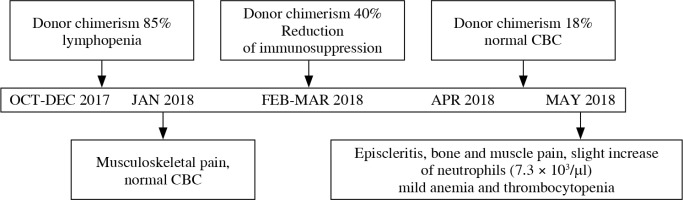
Treatment based on methylprednisolone given in the dose of 8 mg/day and hydroxycarbamide in the dose escalated up to 2000 mg/day resulted in temporary WBC count reduction with musculoskeletal pain resolution. In 4 months, both leukocytosis and polymyalgia recurred with the nadir of the WBC count 106 × 103/µl and only moderate reaction for steroids and HU doses escalation. The patient was eligible for alloHSCT, which was performed in September 2017 from the HLA identical sister of the patient. Reduced intensity conditioning based on fludarabine (total dose 150 mg/m2) and busulfan (total dose 6.4 mg/kg) was applied. As a graft versus host disease (GvHD) prophylaxis, cyclosporine and steroids were administered. In November 2017 the patient developed GvHD skin type in grade II and received methylprednisolone in the dose of 1 mg/kg of body weight. During the period between transplantation and December 2017 polymyalgia was absent and leukopenia in laboratory tests was observed. Between October and December 2017 chimerism analysis revealed stable mixed donor chimerism with 85% donor cells detected in patients’ peripheral blood. At the end of December 2017 musculoskeletal pain, mostly in the lower limbs, appeared followed by the decrease of donor chimerism level to 40% detected in January 2018. Despite rapid reduction of immunosuppression, in April/May 2017 donor chimerism was at the level of 15%. Neutrophil count slightly increased in the blood smear evaluation. Simultaneously bone and muscle pain intensified. Moreover, episcleritis was diagnosed. The clinical course of MPN and GCA with the donor chimerism evaluation is summarized in Figure 2.
Fig. 2
Clinical course of MPN-U and GCA with donor chimerism evaluation after first allogeneic hematopoietic stem cell transplant
Due to the decline of donor chimerism and relapse of symptoms present at the diagnosis, the second transplant was performed in May 2018 with non-myeloablative conditioning (fludarabine 150 mg/m2, cyclophosphamide 1500 mg/m2 and total body irradiation with a dose of 2 Gy). Directly before transplantation no laboratory symptoms of MPN recurrence were observed. Severe musculoskeletal pain of the lower limbs was present until 12 days after alloHSCT. Resolution of symptoms after steroid treatment and recovery of hematopoiesis of donor origin were observed.
Discussion
Myeloproliferative neoplasms are a group of diseases caused by a clonal mutation in precursor myeloid lineage cells. Classification into specific types of MPNs is based on criteria included in the WHO 2016 classification of myeloid neoplasms and acute leukemias [10]. The criteria are mostly based on morphological features of bone marrow and peripheral blood cells but also contain specific genomic mutations. In most cases, ‘driver’ mutations in JAK2, CALR or BCR/ABL1 translocation are present. This facilitates assigning presented symptoms to specific MPN and confirms the clonal nature of cell expansion. Our patient, however, demonstrated none of those in routine tests, which were fluorescent in situ hybridization (FISH) and polymerase chain reaction (PCR). Triple-negative BCR-ABL (–) MPNs comprise a diagnostic challenge and occur in all MPN subtypes with various frequencies. Atypical CML and MPN-U are typically associated with lack of ‘driver’ mutations. Targeted NGS provides support in such cases [11, 12]. This method is a fast and sensitive approach to detect genomic aberrations which otherwise could not be identified. In the described case, demonstration of the presence of heterozygous ASXL1, TET2, SRSF2, CBL mutations in NGS helped to confirm the diagnosis. The relevance of TET2 and ASXL1 mutations lies in affecting epigenetic regulation of specific genes’ expression. They are reported in about 30% of patients diagnosed with aCML or MPN-U and even up to 61% of CMML patients [13]. CBL (targeting the tyrosine-signaling pathway) and SRSF2 (splicing factor) are mainly associated with CMML [14, 15].
The second diagnostic challenge in the described case was overlapping of MPN and autoimmune disease symptoms. High leukocytosis with dominance of neutrophils, anemia and systemic inflammatory symptoms are characteristic for both entities. According to some research, leukocytosis is detected in almost 30% and mild anemia in more than 50% of GCA patients [16]. Moreover, polymyalgia rheumatica, commonly associated with GCA, and GCA itself may imitate other diseases, hampering proper diagnosis. Gonzalez-Gay et al. analyzed data from 206 patients demonstrating PR symptoms, 23 of whom were initially diagnosed with another comorbidity, mainly rheumatic. Furthermore, patients with hematologic neoplasm and PR demonstrated atypical symptoms of PR, such as diffuse aching without any correlation with movement [17]. In our case, symptoms of GCA were also non-characteristic, with a lack of cranial vessels’ involvement demonstrated by headaches, which is present in the majority of patients. Regarding the fact that co-occurrence of MPN with autoimmune disorders is not so rare, the issue of proper interpretation of clinical features and laboratory test results seems very important.
To our knowledge, about 30 cases of co-incidence of GCA or other large vessel inflammatory conditions and myeloid neoplasms have been reported. Most of them concerned patients with MDS, only a few with CMML or essential thrombocythemia (ET) [18-22]. Simultaneous occurrence of hematologic neoplasms and autoimmune disorders could be explained by common factors leading to changes in the immune system. In addition, the primary character of the autoimmune process as the inflammation-driven increased risk of neoplasm development is well known. Anderson et al. analyzed a US medical database with over 13,000 patients with myeloid neoplasms searching for a correlation with rheumatic disorders. The results showed an association between autoimmune disorders and higher risk of myeloid neoplasm development, especially AML and MDS. The most frequently identified autoimmune diseases which may increase the risk of AML and MDS were rheumatoid arthritis, systemic lupus erythematosus, polymyalgia rheumatica, systemic vasculitis, ulcerative colitis and rheumatoid arthritis [23]. Analysis of the Swedish Cancer Registry for patients with MPN diagnosed between 1958 and 2005 demonstrated 20% increased risk of MPN in patients with a history of autoimmune diseases. The most prominent risk was attributable to GCA and Reiter’s syndrome, especially with seronegative types of those diseases [24].
In the pathogenesis of GCA two Th-driven pathways were identified, which involve Th17 and Th1 lymphocytes. CD4 T cells differentiate into Th1 and Th12, which produce interferon gamma and Il-17. These cytokines, in turn, activate macrophages to produce pro-inflammatory cytokines. This initiates systemic and local inflammation [25]. Differentiation of CD4 T cells into Th17 cells is sensitive to steroid treatment but Th1 cells are often resistant and cause disease smoldering [26]. Steroid therapy resolves most symptoms by targeting Th17, but vessel infiltration remains. The vessel involvement is promoted by T lymphocytes, but the inflammation cascade leads to granulocyte and macrophage infiltration. Treatment of large vessel vasculitis is based on steroids or methotrexate and new agents such as tocilizumab [27-29]. We found only one case of successful allogeneic peripheral blood stem cell transplantation in a patient with chronic myelomonocytic leukemia and refractory aortitis described in the literature [30]. The myeloablative conditioning regimen consisted of cyclophosphamide and total body irradiation. In the GvHD prophylaxis methotrexate and cyclosporine were used. The patient developed skin type of GvHD but the procedure resulted in remission of aortitis. That phenomenon was explained by both myeloablation and GvHD occurrence.
In our case, symptoms of autoimmune disorder in the form of polymyalgia also resolved after alloHSCT performed as MPN treatment. Interestingly, as the donor signal decreased within a few months after the procedure, generalized musculoskeletal pain recurred and non-infectious episcleritis was diagnosed. Simultaneously, an increase of leukocytes was observed. This might suggest relapse of MPN as well as GCA because both entities are associated with aberrations in the peripheral blood morphology. Overlapping of symptoms made identification of the real cause of hematological aberrations more difficult. Due to the features of donor stem cell rejection, a second allogeneic transplant was performed with a result similar to the first one. The outcome proved a beneficial effect not only for hematologic neoplasm but also autoimmune disease. This result can be caused by host T-cell depletion and immune reconstitution of donor origin as a result of alloHSCT. Furthermore, GvHD treatment may also play a role in autoimmune process inhibition. Immunosuppressive treatment may lead to impairment of the inflammation cascade and prevent formation of vessels. The pathogenesis of GvHD includes a T-cell-dependent pathway. Triggering of donors’ T lymphocytes by host antigens caused massive inflammatory cytokine production. Immunosuppression used in GvHD prophylaxis and treatment is aimed at Th lymphocytes’ downregulation, which also targets the process of vascular inflammation in GCA.
To conclude, co-occurrence of MPN and autoimmune vasculitis is not very rare. However, overlapping of symptoms could make proper diagnosis hard to establish, especially in atypical variants of the diseases. On the other hand, MPN treatment and alloHSCT may lead to inhibition of an autoimmune process.


