Introduction
Prosthetic valve endocarditis (PVE) is a rare but serious complication of cardiac valve replacement and valve reconstruction surgery, and is associated with high levels of morbidity and mortality. Despite significant advances in understanding the pathogenesis and treatment of this disease process, the incidence of adverse outcomes, including mortality directly related to infection, remains unacceptably high. The risks associated with the technical difficulties of reoperations, especially in patients who underwent coronary surgery in the previous operation with a working LIMA-LAD (left anterior descending artery) graft become even greater [1, 2]. One of the common technical challenges of cardiac reoperations is the dissection and external control of a patent left internal mammary artery (LIMA) graft in patients who have undergone previous coronary artery bypass surgery. Control of this artery becomes necessary when cardioplegic techniques are used for myocardial protection, because blood flowing through a patent graft would otherwise wash away the cardioplegic solution. Mobilization and external clamping of a patent LIMA graft can cause injury to the vessel, leading to adverse short- and long-term outcomes. Angioplasty balloon occlusion of the LIMA graft – an interesting alternative to external clamping – was first described in 2001 by Grinda et al. [3].
Control coronary angiography was performed in all patients over 40 years of age admitted for reoperation. In the presence of previous coronary surgery, in addition to the patency of the grafts, their topographic correlation with the posterior sternal surface and the possibility of damage during re-exploration of the mediastinum were assessed. In the presence of a permeable LIMA graft to the left anterior descending (LAD), after 2016 the method of temporary occlusion with an angiographic balloon catheter was used.
When performing reoperations for PVE, another specific aspect in reoperative cardiac surgery was taken into account – the presence of working bypasses from the previous operation – as the presence of a passable LIMA graft, which is most often anastomosed to the LAD, is a special aspect. It is also taken into account that the difficulties may be on the one hand the risk of injury to the arterial conduit during dissection of the adhesions, and on the other hand the need for temporary occlusion of the LIMA during aortic clamping in order to achieve good myocardial protection and a bloodless operative field.
The options for the surgical team are to work on hypothermia of the fibrillating heart, without aortic clamping, or to dissect a segment of the internal mammary artery (IMA) and temporarily clamp it. In the first variant, the fibrillating heart, even in the conditions of hypothermia, has higher oxygen consumption than in cardioplegic arrest. This poses risks in prolonged operating time. Another inconvenience is the “moving operative field”, as well as the retrograde bleeding from the trunk of the left main coronary artery when working on the aortic valve and the presence of a working, included IMA-LAD graft. In the variant with dissection and direct clamping of the IMA, there is a real risk of injury and compromise of the graft, which is particularly important for the outcome and favorable long-term prognosis after surgery.
Aim
The aim of this study was to compare the data of patients with angiographic balloon LIMA occlusion and those without occlusion in operations related to PVE, and previous coronary surgery with a permeable LIMA graft, determining the degree of safety and benefits of the method.
Material and methods
The study was conducted as an observational study in a single center for cardiac surgery by retrospective analysis of the hospital database. Approval was obtained from the institutional academic board for this study and individual patient consent was waived.
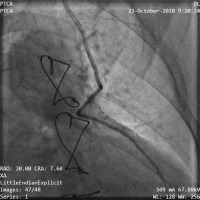
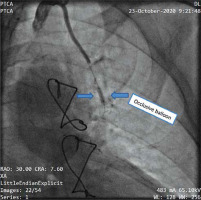
In such cases, for the last 6 years, a method with angiographic balloon occlusion of the LIMA has been used. All patients had previously undergone LIMA grafting of the left anterior descending coronary artery, and, in all cases, preoperative angiography had confirmed the patency of the graft. After signing informed consent forms, the patients were taken to the cardiac catheterization laboratory immediately before reoperation. A common left-femoral approach was used, and systemic heparin (70 IU/kg) was administered. A 6F sheath was placed and an IMA guide catheter was inserted to cannulate the IMA and to obtain posteroanterior and left anterior oblique angiographic views of the IMA graft. The IMA size, estimated visually, varied from 2.0 to 3.5 mm in our patients (Figure 1). A Hi-Torque Balance 0.014-inch coronary guidewire was then positioned into the IMA, followed by an over-the-wire balloon that was 15 mm long with a nominal diameter of 2.0 to 3.5 mm. The balloon was briefly inflated at the nominal pressure (6 atm), and angiography was performed to ensure occlusion of the LIMA graft (Figure 2). The balloon was then left, deflated, in a relatively straight segment of the proximal IMA.
The patients were then transferred to the operation room for routine placement of monitoring lines and anesthetic induction. Re-sternotomy was begun, and the patients were placed on total cardiopulmonary bypass. Aortic cross-clamping and intermittent ante- and retrograde cold-blood cardioplegic arrest were used in all patients for myocardial protection. Deep hypothermic circulatory arrest was not required in any patient. At the time of aortic cross-clamping, the LIMA balloon was inflated at nominal pressure (6 atm) to occlude the IMA. The balloon was deflated at the time of aortic cross-clamp release and before the appointment of protamine, the balloon and the guide are removed. Only the arterial port is left, which is explanted postoperatively. All IMA grafts were found to be patent, with no significant narrowing. The IMA balloon was inserted successfully in all cases, and no complications were encountered during preoperative catheterization. Satisfactory occlusion of LIMA flow with inflation of the endoluminal balloon was seen on preoperative angiography in all patients. Endoluminal occlusion of the LIMA graft was performed intraoperatively in all cases, and no patient required external occlusion of the graft.
This method allows the implementation of optimal control over the IMA, with minimal risk of damage to the vessel. At the same time, secure clamping and good myocardial protection create peace of mind and improve operational results.
Results
In about a quarter of all patients operated on for PVE (25.32%), previous surgery involved the coronary surgery and a working LIMA graft to the LAD was found. In 10 of them (50%) operated on before 2016, the method of angiographic balloon LIMA occlusion was not used, and in the remaining 10 (50%) operated on after 2016, they used this method. This made it possible to divide the patients into 2 groups: group A patients – with LIMA occlusion; and group B patients – without LIMA occlusion). The pre-, intra- and postoperative results were compared and the degree of safety and benefits of the application of the method were studied.
In terms of peri-operative characteristics, the two groups are comparable, without significant differences (Table I).
Table I
Perioperative characteristics of the patients in groups A and B
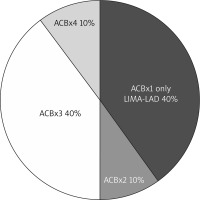
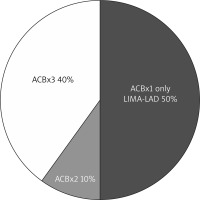
In group A, 30% of patients had active, uncontrolled infection, and in group B, 20%. Also, 30% of the patients in the first group underwent emergency surgery, while in the second group, none did. The data on the bypasses performed in the previous intervention are shown in Figures 3 and 4.
When CPK-MB was monitored immediately after the operation, an increase in the MB fraction of the enzyme to values above 90 U/l was found in 30% of patients in group A and in 50% of patients in group B.
Figure 4
Number of bypasses performed during the previous operation in group B (without LIMA occlusion)
Ten percent of patients in group A and none in group B were in a state of shock on admission to the operating room, and 40% of those operated on in group A and 20% of the control group were in a septic state with uncontrolled infection.
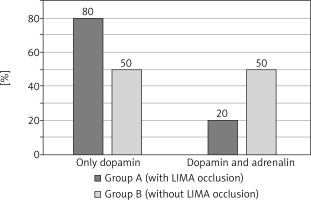
Postoperative complications such as the development of renal, respiratory and heart failure are shown in Figure 5. 80% of patients in group A needed only dopamine infusion and 20% needed the addition of a second catecholamine (adrenaline). In group B, double catecholamine maintenance was needed in 50% of patients (Figure 6).
Figure 5
Preoperative complications in both groups (with and without occlusion)
HF – heart failure, RF – renal failure, RsF – respiratory failure.
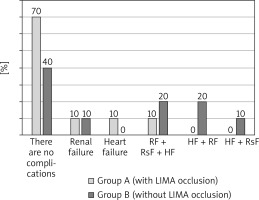
The need for implantation of an intra-aortic balloon pump due to refractory heart failure was registered in 10% of patients in group A and in 20% of patients in group B.
In practice, there was no re-exploration for bleeding, transient disturbance of consciousness, or need for tracheal and gastrostomy in either of the two groups.
In the Mann-Whitney test for comparison of 28 indicators between the two groups, it was found that the average duration of mechanical ventilation in group A was 10.5 hours postoperatively, and in group B it was 12.5 hours. The mean duration of catecholamine infusion in both groups was 3 days. The average stay in intensive care was shorter for patients in group A (2.5 days) than in group B (3.5 days).
In terms of survival, mortality in the group with LIMA occlusion was 0%, while in the group without LIMA occlusion it was 20%.
Conclusions
In 2001, the first publication by Grinda et al. appeared, describing 3 cases of reoperations in patients with previous coronary surgery and a patent LIMA-LAD graft [3] using IMA angiographic balloon occlusion for better myocardial infarction protection and a bloodless operative field. It should be noted that this method is routinely used in our clinic with excellent results.
In about a quarter of all patients operated on for PVE (25.32%), a previous operation was associated with coronary surgery and a working LIMA graft to the LAD was established. Comparing patients with angiographic balloon LIMA occlusion with those without, it was found that in terms of perioperative characteristics the two groups were without significant differences. In the group with LIMA occlusion those with active, uncontrolled infection comprised 30% of patients, and in the control group they made up 20%. Also, 30% of the patients in the first group underwent emergency surgery, while in the second group none did.
When monitoring CPK-MB immediately after surgery, an increase in the MB fraction of CPK to values above 90 U/l was noted in 30% of patients in the group using IMA occlusion, and in 50% of patients in which this method is not used. Ten percent of patients in group A and none of group B were in a state of shock upon admission to the operating room, and 40% of those operated on in group A and 20% of those in the control group were in a septic state with uncontrolled infection.
Eighty percent of patients in group A needed only dopamine infusion and 20% needed the addition of a second catecholamine (adrenaline). In group B, the need for double catecholamine maintenance was noted in 50% of patients.
The need for implantation of an intra-aortic balloon pump due to refractory heart failure was registered in 10% of patients in group A and in 20% of patients in group B.
In practice, there was no revision for bleeding, transient disturbances of consciousness, tracheostomy or gastrostomy in any of the patients in either group.
In the Mann-Whitney test, comparing 28 indicators between the two groups, it was found that the average duration of mechanical ventilation in group A was 10.5 hours postoperatively, and in group B it was 12.5 hours. The mean duration of catecholamine infusion in both groups was 3 days. The average stay in intensive care was shorter for patients in group A at 2.5 days, and in group B it was 3.5 days.
In terms of survival, mortality in the group with LIMA occlusion was 0%, while in the group without LIMA occlusion it was 20%.
The data presented by us agree with those of Theodore Velissaris et al. [4], who followed 9 patients using the LIMA balloon occlusion method. They report no myocardial infarction or cerebrovascular accidents. Patients were on mechanical ventilation for an average of 18 ±5 hours. The average stay in intensive care was 2 days. No false femoral aneurysms or other catheterization complications were reported. Borger et al. [2] and Byrne et al. [5, 6] reported 12.5% of cases of damage to the LIMA graft in an attempt at dissection and external clamping. There was no case of IMA graft damage among the patients we examined.
Our reported results are from the use of the LIMA balloon occlusion method in patients with prosthetic valve endocarditis who are high-risk and complicated patients; nevertheless, the mortality in this group in our study was 0% and no serious complications of the applied method have been registered.
Therefore, we believe that angiographic balloon LIMA occlusion is a reliable, easily applicable and relatively safe technique that improves the surgical results and prognosis of patients in need of reoperative cardiac surgery.